Dental Implants Explained: Benefits, Longevity, and Everyday Care
Dental Implants: What They Are and How They Work
Dental implants have reshaped modern restorative dentistry by offering a fixed, lifelike replacement for missing teeth. Instead of resting on the gums or leaning on neighboring teeth, an implant anchors directly into the jawbone, creating a foundation that can support a crown, bridge, or even a full arch of teeth. For many adults, this approach restores chewing function and a natural smile with reassuring stability.
Outline of this article:
– Part 1: What implants are, components, materials, and the step-by-step process
– Part 2: Core benefits—function, bone preservation, comfort, and quality of life
– Part 3: Longevity—what affects lifetime and the care habits that keep implants healthy
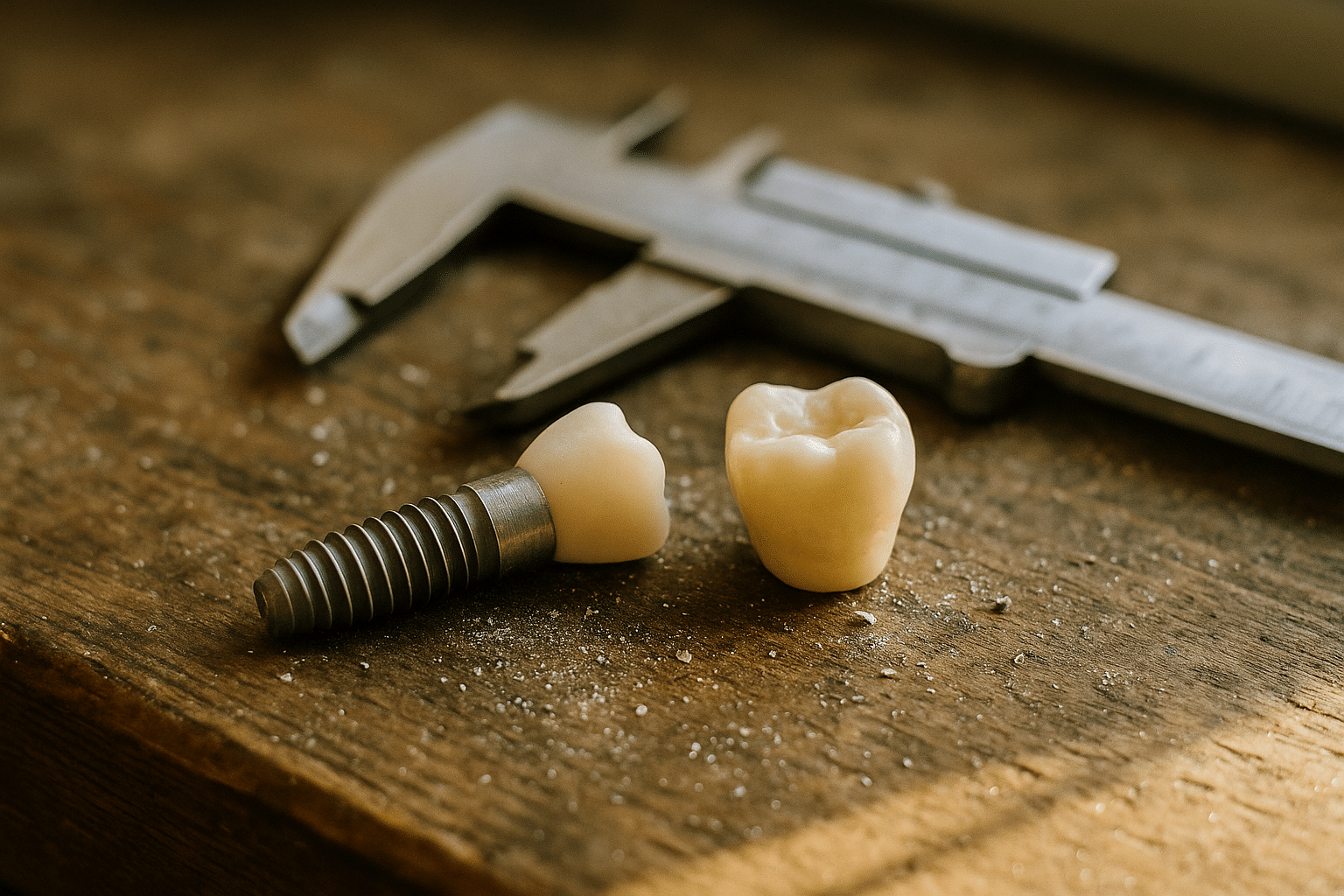
An implant-based tooth replacement typically consists of three parts: the implant body (a small, screw-shaped post placed in the jaw), the abutment (a connector), and the crown (the visible tooth). Most implants are made from biocompatible titanium, a material known for its ability to fuse with bone—a process called osseointegration. Zirconia implants are another option in certain cases, valued for their tooth-colored appearance and bio-inert properties.
From evaluation to final restoration, the process is methodical and personalized:
– Assessment and planning: A clinician reviews medical and dental history, examines gum health, and often uses 3D imaging to map bone quantity and vital structures.
– Site preparation: If bone is insufficient, grafting may be recommended to create a stable foundation.
– Surgical placement: The implant is positioned in the jaw, followed by a healing phase (commonly several weeks to a few months) to allow osseointegration.
– Abutment and crown: Once stable, a custom abutment and crown are attached, completing the new tooth.
Who might be a good candidate? Adults with healthy gums, adequate bone or graftable sites, and a commitment to oral hygiene. Conditions such as uncontrolled diabetes, active gum infections, heavy smoking, or prior high-dose radiation to the jaw require careful evaluation. Certain medications that influence bone metabolism may also affect healing. None of these are automatic exclusions, but they underscore the value of individualized treatment planning.
Alternatives include fixed bridges (which often require reshaping the adjacent teeth) and removable dentures (which sit on the gums). Each option has merits, and a thorough consultation helps align treatment with personal goals, anatomy, and budget. Long-term clinical studies generally report high success rates for implants—commonly above 90% over many years—when case selection, surgical technique, and home care are well managed. That said, success is not guaranteed, and outcomes depend on multiple factors, including gum health and lifestyle habits. Think of an implant as a well-built foundation in a home renovation; it’s designed to last, provided the surrounding structure remains healthy and well cared for.
Benefits of Dental Implants: Function, Health, and Confidence
Implants are often chosen for their ability to mimic the feel and function of natural teeth. Because they integrate with bone, chewing forces are transmitted through the jaw, which can provide a stable, confident bite. Many people report that foods once avoided with removable dentures—like crisp vegetables or chewy grains—return to their everyday menu with implant-supported teeth.
Functional advantages extend beyond comfort:
– Chewing efficiency: Implant-supported teeth can approach the efficiency of natural dentition for many patients, helping support balanced nutrition.
– Speech and stability: A fixed, well-fitted crown does not shift, which can help articulation and reduce the need for adhesives.
Health benefits are a core part of the value proposition. When a tooth is lost, the bone underneath naturally begins to resorb over time due to reduced stimulation. Implants help transmit gentle, functional forces to the bone during chewing, which may help stabilize bone levels around the site compared to non-fixed alternatives. Additionally, because implants do not require reshaping neighboring teeth (as a traditional bridge often does), more of your natural tooth structure can be preserved.
Soft-tissue contours and aesthetics also come into play. A well-designed implant and crown aim to support the gum tissue for a natural emergence profile, blending with adjacent teeth. While artistry and biology both influence the final appearance, many patients find the result reassuringly discreet. On a day-to-day basis, care routines are similar to caring for natural teeth, which can simplify life compared to certain removable prostheses.
From a lifestyle standpoint, implants can contribute to confidence. Eating in company, laughing without worrying about movement, and waking up without removing or reinserting a device are conveniences that many users appreciate. Over the long term, implants can be cost-effective when they remain healthy, especially since they do not rely on adjacent teeth for support. That said, they are not a one-size-fits-all solution. Considerations include time for healing, surgical candidacy, and the need for ongoing maintenance. A transparent discussion with your clinician regarding expectations, timelines, and alternatives ensures you choose an option aligned with your priorities.
It’s helpful to remember that every restorative pathway has trade-offs:
– When a bridge may be preferable: If neighboring teeth already need crowns or if surgery is not advisable.
– When a removable option may be practical: When multiple teeth are missing and rapid, non-surgical replacement is preferred, or when budget is the immediate limiting factor.
– When implants are appealing: For fixed stability, bone-level support, and preservation of adjacent teeth.
In short, implants are a well-regarded solution that blend engineering and biology to restore function and appearance, provided the surrounding tissues are kept healthy and habits support long-term success.
Lifetime and Care: How Long Implants Last and How to Protect Them
How long do dental implants last? With good planning and consistent care, they can serve for many years—often decades. It’s helpful to think in terms of components. The implant body (in the bone) is designed for long-term service. The crown, being the visible and working surface, experiences wear and may need replacement after a period that commonly ranges around 10–15 years, depending on bite forces, materials, and care. The abutment, the connector between implant and crown, occasionally requires replacement if damaged or if the restoration is updated.
Several factors influence longevity:
– Gum health: Healthy, inflammation-free gums and adequate bone support are foundational.
– Bite forces: Clenching or grinding (bruxism) can stress implants; a night guard may be recommended.
– Hygiene habits: Daily biofilm control is essential to reduce the risk of peri-implant mucositis and peri-implantitis.
– Systemic health and lifestyle: Tobacco use, uncontrolled diabetes, and certain medications can affect healing and long-term stability.
Daily care is straightforward but precise:
– Brush twice daily with a soft-bristled brush and a low-abrasive paste to avoid scratching the crown surface.
– Clean between the implant crown and neighboring teeth daily. Interdental brushes with nylon-coated wires, floss threaders, or water flossers can help remove plaque where brushes cannot reach.
– Rinse as advised by your clinician, especially if gums are sensitive or a new implant is healing.
– Avoid using teeth to open packages, and reduce biting on very hard items like ice or unpopped kernels.
Professional maintenance complements home care. Regular checkups—often every six months, or more frequently if recommended—allow your dental team to measure gum health, monitor bone levels with periodic imaging, and remove hardened deposits with techniques suited to implant surfaces. Early detection matters: bleeding around an implant, persistent bad taste, gum swelling, or loosening of a restoration are signals to seek prompt evaluation. Inflammation limited to the soft tissue (peri-implant mucositis) is generally manageable when caught early; inflammation with bone loss (peri-implantitis) requires more advanced care.
Protective strategies help extend service life:
– Wear a night guard if you grind or clench; distributing forces can reduce mechanical stress.
– Use a sports mouthguard during contact activities.
– If dry mouth is a concern, consider saliva-supporting measures and frequent hydration to help control biofilm and acidity.
– Discuss any new medications or health changes with your clinician since they can influence tissue responses.
With thoughtful maintenance, many implants remain stable for decades, offering dependable function and appearance. The key is partnership: you handle daily care and protective habits, while your dental team monitors the supporting tissues and hardware. Together, that combination keeps your implant performing like a quiet, reliable cornerstone in your smile.
Conclusion
Dental implants provide a stable, natural-feeling way to replace missing teeth, helping you chew comfortably, protect jawbone, and preserve neighboring teeth. By understanding how implants work, what benefits they offer, and how to care for them, you can make a confident, informed decision. If you are considering treatment, an individualized assessment—covering gum health, bone structure, and lifestyle—will clarify whether implants align with your goals. With smart habits and regular professional care, implants can be a long-lasting investment in your health and daily comfort.


