Dental Implants: Benefits, Longevity, and Everyday Care Guide
Outline
We’ll start with what dental implants are, how they’re placed, and who typically qualifies. Then we’ll unpack the key benefits—chewing function, comfort, bone preservation, and how implants interact with neighboring teeth. Finally, you’ll find realistic longevity ranges and a clear care plan you can use daily, plus maintenance timelines that help extend implant life. Along the way, we’ll point you to trusted clinical guidance and product resources, and share a real‑world example to bring the details to life.
Introduction
Missing teeth change far more than a smile—they can affect speech, chewing confidence, and even the shape of your face. Dental implants offer a stable, lifelike replacement that many people find easy to live with. This guide explains how implants work, the advantages people often experience, and what truly influences longevity. You’ll also get a practical daily care checklist and maintenance schedule so you can protect your investment with routines that fit real life.
Dental implants explained: parts, process, candidacy, and alternatives
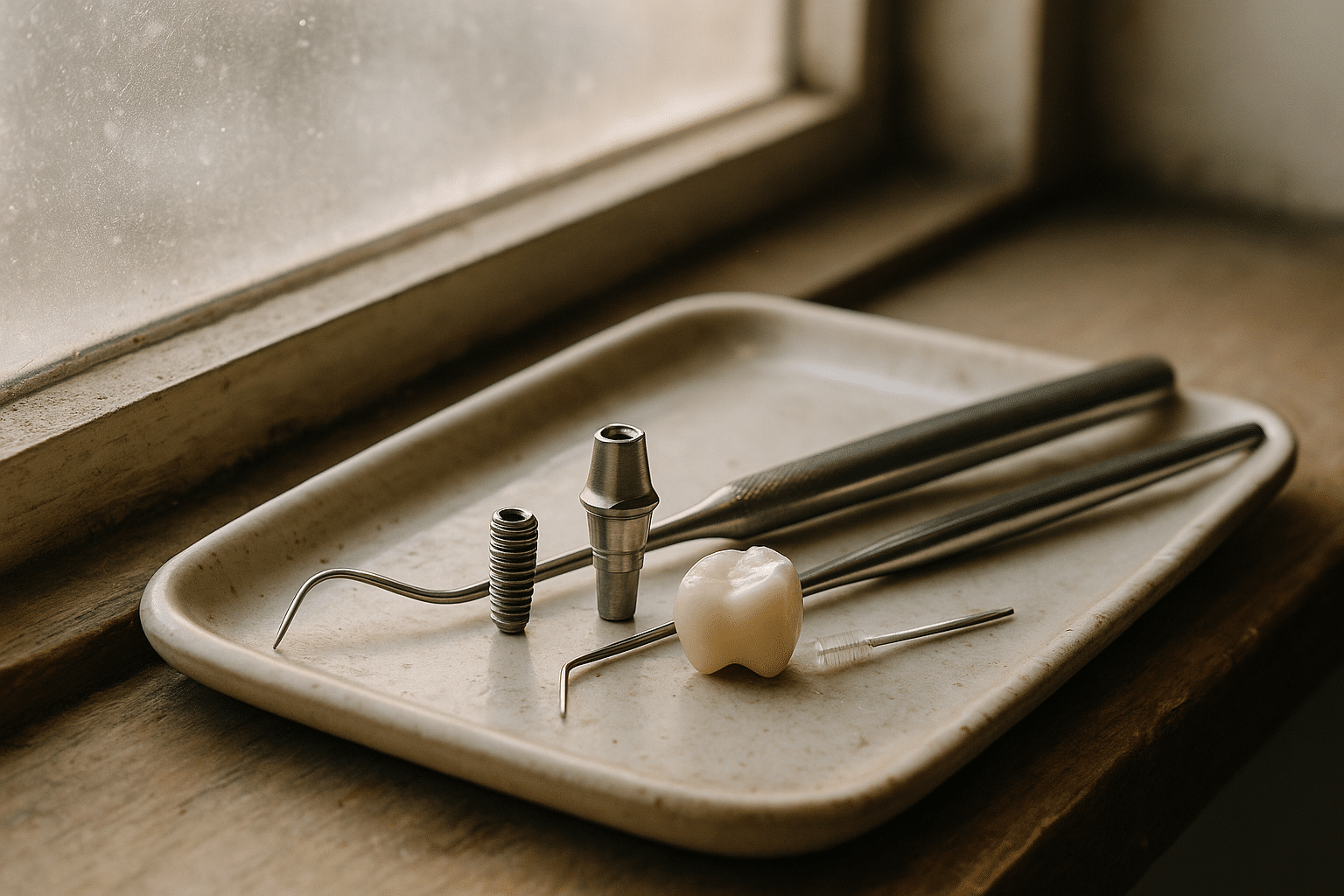
What is a dental implant? In everyday use, “dental implant” refers to a small post (usually titanium) placed in the jawbone, a connector called an abutment, and a custom crown on top. Together they replace a missing tooth root and the visible tooth. The American Academy of Periodontology notes that endosteal implants (within the bone) are the most common, while subperiosteal implants (on top of the bone) are less common and used in specific cases. You may also hear about zygomatic implants in complex upper‑jaw cases. ([perio.org](https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/?utm_source=openai))
How placement works (typical single‑tooth timeline): evaluation and planning (including 3D imaging), surgical placement of the implant, a healing period to allow bone fusion (osseointegration), then abutment and crown placement. The U.S. Food and Drug Administration (FDA) emphasizes that overall health, smoking status, and adherence to oral‑hygiene instructions influence healing and success; the healing phase can take several months before a final crown is attached. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
Who’s a candidate? Healthy gums, sufficient bone, and good daily oral care habits are important. Periodontists (gum specialists) and prosthodontists (restoration specialists) often collaborate on planning, especially when bone grafting or sinus lifts are needed to support an implant. The AAP provides an accessible overview of candidacy and common adjunctive procedures like sinus augmentation and ridge modification. ([perio.org](https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/?utm_source=openai))
Provider training matters. The American College of Prosthodontists encourages patients to ask about a dentist’s credentials and experience, and highlights when referral to a specialist is appropriate—especially for complex cases. ([prosthodontics.org](https://www.prosthodontics.org/about-acp/position-statement-dental-implants/?utm_source=openai))
Costs and insurance at a glance (United States): Single‑tooth implant therapy (implant + abutment + crown) commonly ranges a few thousand dollars. Delta Dental lists $2,800–$5,600 for a single implant (without benefits), while consumer finance guides like Investopedia report $3,000–$6,000 per tooth and note that some plans cover a portion (often up to 50% for major services). Use your insurer’s estimator tool and request a pre‑authorization to avoid surprises. ([deltadental.com](https://www.deltadental.com/us/en/protect-my-smile/procedures/dental-implant/treatment-cost.html?utm_source=openai), [investopedia.com](https://www.investopedia.com/how-to-get-dental-implants-covered-by-insurance-8580639?utm_source=openai))
Implants vs. bridges vs. dentures
Use this quick comparison when exploring options with your dentist.
| Feature | Single Implant | Fixed Bridge | Removable Partial/Full Denture |
|—|—|—|—|
| Chewing stability | High; feels anchored | High, but relies on adjacent teeth | Moderate; may shift |
| Affects adjacent teeth | No preparation needed | Neighboring teeth usually crowned | Minimal, but clasps may contact teeth |
| Bone preservation at missing site | Helps maintain bone | Does not stimulate bone | Does not stimulate bone |
| Esthetics | Highly realistic | Realistic | Varies with design |
| Typical timeline | Months (healing + restoration) | Weeks | Weeks |
| Daily cleaning | Brush + interdental care around implant | Brush + floss threaders/bridges | Removal for cleaning; soak as advised |
| Longevity potential | Many years with care | Years; subject to abutment tooth health | Years; may need relines/replacement |
| Common add‑on procedures | Bone graft, sinus lift (as needed) | None specific | Tissue conditioning, relines |
| Insurance coverage | Varies; often partial | Often partial | Often partial |
| Surgical requirement | Yes | No | No |
For implant benefits and risks (including nerve injury, sinus issues, screw loosening, and infection), see the FDA’s patient page. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
If you’re ready to focus on upkeep, jump to the Longevity & Everyday Care section below for a checklist you can start using right away.
The benefits of dental implants—and why many patients choose them
Function and confidence. Many patients choose implants for chewing comfort and speech clarity. The FDA lists practical benefits such as restored chewing, improved appearance, stability of adjacent teeth, and quality‑of‑life improvements. These are the everyday wins that help implants feel like part of your mouth rather than something you constantly manage. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
Bone preservation. Implants transmit chewing forces to the jawbone, which helps reduce bone loss at the site of a missing tooth—a difference you’ll notice over years, especially in the back of the mouth where chewing forces are higher. The FDA also notes this advantage explicitly. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
Tooth‑conserving replacement. Because implants stand independently, neighboring teeth typically don’t require reshaping for crowns (unlike many traditional bridges). The AAP overview explains common indications and when single, multiple, or full‑arch implants enter the picture. ([perio.org](https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/?utm_source=openai))
Durability supported by long‑term data. Long‑horizon studies in peer‑reviewed journals track high implant survival, especially when patients attend maintenance visits. For example, a 10‑year analysis of full‑arch rehabilitations reported a cumulative implant survival rate above 96%. A 25‑year cohort under supportive implant therapy reported 95% implant survival with consistent professional care—underscoring the value of recall and hygiene. ([onlinelibrary.wiley.com](https://onlinelibrary.wiley.com/doi/abs/10.1111/clr.13411?utm_source=openai))
But “survival” isn’t the whole story. Some patients experience technical or biological complications (like ceramic chipping, screw loosening, mucositis, or peri‑implantitis) that require maintenance even when the implant remains in place. Editorial commentary in the European Journal of Oral Sciences reminds clinicians and patients to look beyond survival rates and consider real‑world complications and upkeep. ([onlinelibrary.wiley.com](https://onlinelibrary.wiley.com/doi/full/10.1111/eos.12543?utm_source=openai))
What experts say about maintenance. The American College of Prosthodontists led clinical practice guidelines on recall and at‑home care for implant‑borne restorations. Media coverage of these guidelines distilled the patient takeaway: “The patient needs to be in an active partnership with their prosthodontist, dentist, and hygienist.” Another ACP contributor noted that people outside maintenance programs face a markedly higher chance of losing implants over time. Keep the partnership strong with scheduled visits and daily care. ([aegisdentalnetwork.com](https://www.aegisdentalnetwork.com/news/2017/04/6/dental-implants-crowns-bridges-and-veneers-8-tips-from-prosthodontists-to-avoid-failures?utm_source=openai), [pubmed.ncbi.nlm.nih.gov](https://pubmed.ncbi.nlm.nih.gov/26896518/?utm_source=openai))
Real‑world example (name changed for privacy): After a bike mishap, Priya lost an upper premolar and chose an implant. She appreciated that her adjacent teeth stayed untouched and that chewing felt natural once the crown was placed. At first she struggled to clean around the implant; her hygienist switched her to a compact interdental brush and suggested a water flosser. Priya now books three‑month cleanings during allergy season (when her gums tend to be inflamed) and six‑month intervals the rest of the year—an approach that’s kept her implant comfortable for years.
Helpful resources to explore: See the ADA’s patient page on implants and the AAP’s procedure guide to understand candidacy and steps; both are written in accessible language and include visuals. ([mouthhealthy.org](https://www.mouthhealthy.org/all-topics-a-z/implants?utm_source=openai), [perio.org](https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/?utm_source=openai))
Longevity and everyday care: realistic timelines, risk factors, and a maintenance plan
How long do dental implants last? With healthy gums and consistent professional care, many implants function for decades. Long‑term cohorts show high survival when patients stick with supportive implant therapy (SIT). One 25‑year follow‑up reported 95% implant survival among SIT‑compliant patients and highlighted that most implant losses were linked to uncontrolled peri‑implantitis—an infection‑driven breakdown of supporting bone. ([onlinelibrary.wiley.com](https://onlinelibrary.wiley.com/doi/full/10.1111/cid.12944?utm_source=openai))
Know the major risks—and what you can control. The FDA lists smoking, uncontrolled diabetes, and difficulty cleaning the implant area among factors that can jeopardize outcomes. The European Federation of Periodontology (EFP) issued 2023 clinical guidelines stressing prevention and a structured supportive care program to monitor peri‑implant tissue health after loading. Together, these reinforce a central message: daily plaque control and regular check‑ins are non‑negotiable. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai), [efp.org](https://www.efp.org/news-events/news/efp-publishes-guideline-on-the-prevention-and-treatment-of-peri-implant-diseases-30965/?utm_source=openai))
Peri‑implant disease, explained. The AAP and EFP’s 2017 World Workshop introduced standardized definitions for peri‑implant health, peri‑implant mucositis (reversible soft‑tissue inflammation), and peri‑implantitis (inflammation with progressive bone loss). These definitions help your dental team diagnose early and act before bone changes become advanced. ([perio.org](https://www.perio.org/research-science/2017-classification-of-periodontal-and-peri-implant-diseases-and-conditions/?utm_source=openai))
Maintenance intervals and what happens at visits. ACP guidance recommends tailoring recalls to risk—often every 2–6 months for higher‑risk patients (history of periodontitis, smoking, dexterity challenges) and semiannual visits for lower‑risk patients. Professional maintenance typically includes checking tissue health (probing depths, bleeding), assessing occlusion, reviewing self‑care, selective debridement with implant‑safe instruments, and periodic radiographs (about every 1–2 years, or sooner if concerns arise). ([prosthodontics.org](https://www.prosthodontics.org/about-acp/position-statement-maintenance-of-full-arch-implant-restorations/?utm_source=openai))
Daily care checklist (save this):
– Brush twice daily with a soft brush; many people prefer a powered model with a pressure sensor to avoid overbrushing. The ADA explains what its Seal of Acceptance means and lists powered brushes that meet evidence‑based criteria; reviewers at People independently tested electric brushes and described models with helpful coaching features. ([ada.org](https://www.ada.org/resources/ada-library/oral-health-topics/toothbrushes/?utm_source=openai), [people.com](https://people.com/best-electric-toothbrushes-11772585?utm_source=openai))
– Clean between teeth and around the implant daily. The ADA’s guidance on floss and interdental cleaners explains why these tools matter for plaque control and gum health. Water flossers can help if threaders are difficult to use. ([ada.org](https://www.ada.org/resources/ada-library/oral-health-topics/floss/?utm_source=openai))
– Use a non‑abrasive toothpaste and an alcohol‑free antimicrobial rinse if your clinician recommends one (especially if you are prone to inflammation).
– Protect your implant from excess force: if you clench or grind, ask about a custom night guard; avoid chewing ice and very hard foods.
– If you smoke or vape, get support to quit; your dental and medical teams can suggest programs and nicotine‑replacement options. The FDA cautions that smoking can delay healing and reduce long‑term success. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
Care milestones and monitoring
| Milestone | What to expect | Why it matters |
|—|—|—|
| Surgery day | Implant placed; follow post‑op instructions | Sets up healthy healing |
| 1–2 weeks | Suture removal, soft‑tissue check | Confirms early healing |
| 6–12 weeks | Osseointegration check (varies by case) | Verifies stability before loading |
| Abutment/crown day | Final bite and hygiene instructions | Prevents overload; supports cleaning |
| 1–3 months post‑crown | First maintenance visit | Early detection of irritation |
| Every 3–6 months | Pro cleaning, tissue check, occlusion review | Controls plaque, monitors bite forces |
| Every 12–24 months | Radiographs as indicated | Tracks bone levels |
| Any time | Report looseness, pain, swelling promptly | Early intervention prevents escalation | ([prosthodontics.org](https://www.prosthodontics.org/about-acp/position-statement-maintenance-of-full-arch-implant-restorations/?utm_source=openai))
Costs over time—and budgeting smartly. National guides estimate single‑tooth implant therapy totals commonly in the $2,800–$6,000 range (geography and complexity matter). Insurers like Delta Dental host local cost estimator tools; consumer finance sources suggest confirming whether your plan covers implants as a major service and obtaining pre‑authorization. If you need a powered brush or water flosser, consider models with the ADA Seal, or read independent reviews to match features with your needs and budget. ([deltadental.com](https://www.deltadental.com/us/en/protect-my-smile/procedures/dental-implant/treatment-cost.html?utm_source=openai), [investopedia.com](https://www.investopedia.com/how-to-get-dental-implants-covered-by-insurance-8580639?utm_source=openai), [ada.org](https://www.ada.org/resources/ada-library/oral-health-topics/toothbrushes/?utm_source=openai), [people.com](https://people.com/best-electric-toothbrushes-11772585?utm_source=openai))
Personal example: Miguel, a night‑shift nurse, received a lower‑molar implant. He struggled to floss consistently after 12‑hour shifts, and mild bleeding developed at three months. His hygienist switched him to a compact water flosser for the nightstand and a slim interdental brush for his locker. He also began wearing a night guard (he clenches during stressful weeks). At his next visit, bleeding had resolved—and his bite felt better, too.
Bottom line: Think of your implant like a precision joint. It can do exceptional work for a very long time, but only if you keep it clean, avoid overload, and let professionals inspect and fine‑tune it regularly.
Comparison table: What matters most when choosing an option
| Factor | Why it matters | Implants | Bridges | Dentures |
|—|—|—|—|—|
| Preserves jawbone at site | Helps facial shape over time | Yes | No | No |
| Involves surgery | Affects recovery, cost | Yes | No | No |
| Uses adjacent teeth | Impacts tooth structure | No | Yes (crowns) | No |
| Chewing strength | Daily function | High | High | Moderate |
| Comfort/stability | Everyday confidence | High | High | Variable |
| Cleaning routine | Daily time/effort | Like natural tooth + interdental | Floss threaders | Remove/soak |
| Typical timeline | Planning to final | Months | Weeks | Weeks |
| Long‑term maintenance | Visits, repairs | Hygiene + recalls | Abutment tooth health | Relines/repairs |
| Insurance variability | Out‑of‑pocket impact | Often partial | Often partial | Often partial |
| Upfront cost (US) | Budgeting | $2.8k–$6k/tooth typical ranges | Varies by span | Varies (often lower) ([deltadental.com](https://www.deltadental.com/us/en/protect-my-smile/procedures/dental-implant/treatment-cost.html?utm_source=openai), [investopedia.com](https://www.investopedia.com/how-to-get-dental-implants-covered-by-insurance-8580639?utm_source=openai))
Conclusion
Dental implants can restore chewing comfort, protect jawbone volume, and deliver a natural look—advantages many people value every day. Equally important, long‑term success is a team effort: consistent home care plus risk‑based professional maintenance dramatically improves the odds that your implant will serve you for years. Use the checklists above to start strong, ask your dentist for a written maintenance plan, and keep an eye on small changes so issues are addressed early. When you’re ready, book a consultation with a periodontist or prosthodontist to tailor options, costs, and timelines to your goals and health profile. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai), [perio.org](https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/?utm_source=openai), [prosthodontics.org](https://www.prosthodontics.org/about-acp/position-statement-maintenance-of-full-arch-implant-restorations/?utm_source=openai))
Dental Implants: Frequently Asked Questions
Do dental implants set off airport scanners or interfere with MRI?
Implants are typically fine at airport security. For imaging, the FDA advises telling technicians you have an implant because it can distort MRI or X‑ray images; adverse events are not commonly reported. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
Is there a strict age limit for getting an implant?
No. Overall health, gum condition, and bone availability matter more than age. Your dentist will assess risk factors and, if needed, coordinate grafting or staged treatment. ([perio.org](https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/?utm_source=openai))
How painful is the procedure and recovery?
Most patients describe pressure and soreness for a few days, managed with over‑the‑counter pain relief and careful hygiene. Your clinician will provide specific post‑op instructions for comfort and healing. ([fda.gov](https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know?utm_source=openai))
What’s the maintenance schedule after I get my crown?
Expect a first check around 1–3 months, then recalls every 3–6 months based on risk, with radiographs about every 1–2 years or sooner if concerns arise. ([prosthodontics.org](https://www.prosthodontics.org/about-acp/position-statement-maintenance-of-full-arch-implant-restorations/?utm_source=openai))
Which toothbrush or flosser should I buy?
Look for the ADA Seal of Acceptance to confirm safety and effectiveness; independent testers also review models for features like pressure sensors and timers. Choose what fits your dexterity and budget. ([ada.org](https://www.ada.org/resources/ada-library/oral-health-topics/toothbrushes/?utm_source=openai), [people.com](https://people.com/best-electric-toothbrushes-11772585?utm_source=openai))
Will insurance help pay for implants?
Coverage varies widely. Some plans cover implants as a major service (often around 50% up to plan limits). Always request a pre‑authorization and use your insurer’s local cost estimator. ([investopedia.com](https://www.investopedia.com/how-to-get-dental-implants-covered-by-insurance-8580639?utm_source=openai), [deltadental.com](https://www.deltadental.com/us/en/protect-my-smile/procedures/dental-implant/treatment-cost.html?utm_source=openai))


